Disarming Cancer's Immune Evasion, Owkin Doses First Patient With AI-Optimized Therapy
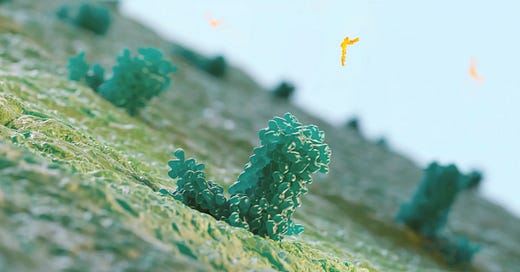
Owkin has entered the clinic with a first-in-class EP2/EP4/DP1 triple inhibitor designed for solid tumors.
After May 2024 expansion of its oncology pipeline through a licensing agreement with Idorsia and the development of a dual EP2/EP4 inhibitor, Owkin has now entered the clinic with OKN4395—a first-in-class EP2/EP4/DP1 triple inhibitor designed for solid tumors.
The first patient in the INVOKE trial was dosed on January 22, 2025, marking the start of a stu…